
Several major data breaches have made the news. And millions of medical records have been breached.
It’s bad enough knowing your credit card information could be out there, but access to medical records is an invasion of privacy. Yet that’s exactly what’s happening — and it’s not always illegal. In fact, some health providers are giving tech giants access to patients’ medical data. The implications of patient data being stolen, shared, and sold are far-reaching, from stolen identities to skyrocketing insurance premiums. Medical Data Breaches On the Rise
Who Has Access to Your Personal Health Information?
Protecting Your Personal Health Information
“If you believe that an online company that is not covered by HIPAA, such as a message board, has shared your health information in a way that conflicts with their privacy policy on their website, you can file a complaint with the Federal Trade Commission.” What Your Doctor Can Do to Protect Personal Health Information
As more healthcare providers adopt cybersecurity frameworks, medical records will hopefully become less vulnerable to theft. In the meantime, consumers must stay vigilant in monitoring their medical records for signs of identity theft and demanding transparency from healthcare providers who share their data with third parties.
0 Comments

By Madeline Miller
Those within the dentistry profession may have noticed that the service doesn’t always promote positive reactions in people. The cliché is that a trip to the dentist is something to be feared. This may be an over-embellishment, but the pervading reputation is clear. The narrative needs to be changed, and dental practices can take ownership of changing that reputation. And it all starts with the dental practice reception – the welcoming arena for those on a trip to the dentist. The atmosphere and environment created by reception is the first impression patients will get on the trip to the dentist, so it needs to be a good one. Here are some key tips to making your practice a welcoming place. Create a welcoming environment Cold and clinical colors don’t radiate warmth, so things can easily be changed by adding a bit of color, and having soft furnishings that add warmth and friendliness to the environment will go a long way to setting visitors at ease. Avoid silence if at all possible, so have a bit of music playing gently in the background, and provide an array of magazines and newspapers for the adults, and a collection of toys and games for younger visitors to the practice. Think carefully about what makes a welcoming atmosphere, and you will quickly understand that it is the small touches, rather than the grand gestures, which do this.
Hire warm and welcoming staff
Many people who visit the dentist do so on edge. So, what is the last thing they want to be faced with that reception staff who show no empathy to their unease. A welcoming smile and kind words upon arrival make a huge difference, as it does in any service profession, so make sure you are not missing out on repeat customers by not having reception staff who are welcoming and friendly in their dealings with patients. Training can be provided, of course, but these considerations should be built into your recruitment processes too. Phone manner is just as important, because if this manner is abrupt and cold, then you may fail to attract the patient through the door in the first place. This issue is regularly cited as a major contributing factor in customer retention, so don’t underestimate the importance of having staff who get what it means to be working in a dental practice. Yes, you are a medical service, but putting your patients at ease should be among your highest priorities. Provide flexible payment options Dental care is expensive for people, so give them options to make those payments. Not only are many people uneasy on a trip to the dentist, but they are also fearful that it’s going to break the bank, so be extremely up front with costs too, and have total transparency in the cost of various services, itemizing bills and providing flexible options to make repayments. In short, be understanding of different patients’ needs. Consider that paying up front is not an option for everybody, so offer solutions that work for as many people as possible.
Use an effective scheduling system
One of the bugbears of patients is that they can arrive at the practice for their appointment, only then finding themselves having to wait for an hour. Nothing puts people on edge like this, and certainly won’t help in retaining patients. The first thing to do is make sure you employ an effective scheduling system, and don’t try to pack patients in too tightly. You may think you are making more money this way, but the bottom will soon fall out of your business when your reputation of rushing the job and leaving people waiting gets around. Instead, allocate plenty of time between appointments, automate your system with automatic text alerts to let patients know if you are running behind schedule, and train your staff in how to effectively deal with patients who find themselves having to wait. All of this helps greatly in retaining business. Madeline Miller is a health writer at Paper fellows and Boomessays Reviews with a particular interesting in the art of communication. She is a regular writing contributor at Assignment writing service. 
By Sara Sparrow
Parenting is always a tricky path, no matter what your family looks like. However, you will face more challenges if your child has faced trauma in the past. This changes the way you'll interact with them and give them the care that they need. Here's what you need to know about adapting your parenting style to help your child thrive after a traumatic experience.
What Is Trauma? Firstly, you should have an understanding of what trauma means for a child. Children are resilient, and there are some experiences that will be anxiety inducing for them, such as being left at school for the first time. However, these are experiences that help them learn and grow. There are some events though, that will have a bigger impact on a child and affect them negatively. Trauma will come about differently for each child, but common traumas include:
The Effects Of Trauma Just like in adults, the effects of trauma are varied in children. These effects can be grouped into four different categories, as follows: Physical: Inability to control physical reactions to stress, chronic illness Mental: Difficulty in learning and concentrating, and switching from one activity to the other. Impaired memory is another key effect of trauma. Emotional: Low self esteem, feeling unsafe, trouble with making friends, trust issues, depression, anxiety, and so on. Behavioral: Substance abuse, lack of impulse control, fighting, and aggression. Helping A Child Who Has Been Through Trauma So, how can you help a child who has been through trauma? There are a few things you should remember, as you'll need to adapt your parenting style to help your child.
Understand They Aren't 'Misbehaving'
It's so easy for a child to be labeled as a 'troublemaker' when they've been through trauma. This is because they had to learn certain behaviors in order to get through the traumatic time in their lives. These behaviors are very much like a reflex, and will come about without the child thinking about it. They may be safe now in your home, but their brain won't have processed that right away. For example, trauma triggers are events that remind the child of the trauma they went through. When they experience this, may either 'fight', take 'flight', or freeze. To you, that can look like they're fighting with you, defying you, or not listening. Understanding these responses is key to caring for such a child. Be Available To Them Your child may not have had positive adult attention before, but you'll want to show them that you're there for them, no matter what. Younger children may want extra attention and hugs, while older children may just want to spend time as a family. Ensure that you're emotionally and physically available to them. Be Consistent Creating a routine for your child will help them recover from the events they've been through, especially if they didn't experience consistency in the past. If any new events or changes are coming up, prepare your child in advance for them. Listen To Their Feelings If your child wants to talk about their feelings, allow them a safe space to do so. Show them it's ok to be dealing with complicated feelings, even though they're now in a safe place. Give Some Control Allowing children some control can help them, when they were used to turbulent living conditions before. Give them age appropriate choices so they can regain that sense of control. Be Patient It may take some time for your child to come to terms with what happened to them. It may take a while for them to fully trust that they are safe. Take everything at their pace, and show them that you're ready and willing to help them through it. Parenting a child who has been through trauma can be challenging, but if you take it slow and show your child you're there for them, you can help them get through it and be happy and healthy. About the author: Sara Sparrow is a health writer with Thesis writing service and Essay services, where she focuses on children's health. She also contributes to sites like Ox Essays. 
By George J. Newton
The last two years have been full of endless worldwide issues, negative mindsets, and life interruptions. We have all definitely been impacted in a variety of ways due to the state of our world. These disturbances have likely affected your mental health and the mental health of those around you. Everyone on this planet has a difficult, unpredictable life. This reality makes mental health awareness a high priority. If you are struggling to maintain your mental health, it’s time to change your approach to caring for yourself. Here are 4 ways you can shift your approach to mental health this year. Stay Active Exercise is a wonderful type of selfcare, and is important for your overall health. Any type of exercise is beneficial to you both mentally and physically. When we exercise, endorphins are released, along with other chemicals associated with happiness such as serotonin. Releasing these chemicals helps individuals achieve a balance of essential hormones. Lack of exercise will cause a deficiency in these chemicals, which will damage one’s mental health overtime. While you don’t have to become an athlete to use this mental health boosting method, try to fit in 30 minutes of physical activity in your schedule daily. It can be as simple as a walk, yoga session, mini dance party in your room, or quick gym session. “Those who prioritize fitness develop larger brain volume. This factor is associated with stronger cognitive functioning amongst people of all ages, but especially adults,” concludes Callie Ponce, mental health blogger at Writemyx.com and Australia2write.com. Proper Nutrition Though ensuring your diet is balanced is often tricky, it is an excellent way to prioritize your wellbeing. When we receive the correct amount of the different types of nutrients, we can thrive in mental and physical areas. Proper nutrition allows the brain to fully develop and perform at the desired level. Those with nutrient deficiencies will endure harmful impacts to the structure and function of their brain. Poor nutrition leads to low academic performance, memory loss, and higher rates of illness and disease. If you have an extremely unhealthy diet, it's time to rethink your meal choices. You should be eating protein, greens, fruit, dairy, carbs, and vitamins to achieve your health goals. Obtaining a balanced diet and receiving proper nutrition will help boost the state of your mental health.
Connecting With Others
During stressful times, connecting with others experiencing similar situations is crucial. Over the last two years, we have all faced our fair share of hardships. Mental health is something every human on this planet has. Nobody can ever have perfect mental health because that is an unrealistic outcome. This is a part of life we can all understand and relate to. When you are struggling mentally, reaching out to friends, coworkers, family, your significant other, and others can make a positive impact. When we can connect and empathize with others and their experiences, we feel understood. In periods of low mental health, it’s common for individuals to feel alone. The truth is we all struggle and have hit rock bottom at some point. “Society is slowly starting to shine light on mental health awareness. This change is laying out a foundation for a future where mental health is seen as an important part of one’s entire wellbeing,” shares Sonia Quinn, journalist at Originwritings.com and Britstudent.com. Making Time For Things You Enjoy Most people are constantly busy trying to make ends meet and get tasks done. When we overfocus on other parts of life, forgetting about doing things we enjoy is a common occurrence. Engaging in hobbies and making time for your favorite activities is one way you can strengthen your mental health. Doing things you love will decrease stress, and put you in a happy mood. Sports, music, art, hikes, and other activities are ways people can escape from life pressure and take a well deserved break. So no matter how busy you are with other responsibilities, try to fit in a few hours a week to do the things that make you happy. These 4 methods will help you shift your approach to mental health this year and for years to come. Investing time into your mental health will be highly beneficial and pay off in the long run. Writer George J. Newton works as a business development manager at both Write my literature review and Dissertation writing service. George has perfected resolving arguments after being with his wife for ten years. He also works for Custom coursework. 
By Dana Corriel MD
Board Game Benefits Board games are fun, first and foremost. My words are always met with pleasure when the words, “Let’s play!” escape my lips. The announcement is usually followed by the loudly happy rummaging through the chest of games, and a big, wide smile appears as they finally find the winner- the chosen one. But board games have health benefits, too. The following are eight ways in which board games teach our children valuable life lessons: 1. They make us happy Engaging in a game stirs up our inner competition, and pushes us to strive towards a goal. This releases endorphins and gives us something that occupies our time, and which serves a purpose (to win the game, and have fun while getting there). 2. They teach children how to lose It sucks to lose. But what’s worse is winning to a sore loser. When we win fair and square, we want to enjoy that moment, and not have to explain our win, or console others. Children who play regularly, and are challenged, learn that it’s ok to be on the losing end sometimes. And let’s face it, losing serves as a motivating drive to get even better and that’s a lesson that’s ultra important for our kids. 3. They help children expand their planning skills Games almost always require thinking ahead. Children must form these thoughts in their heads, plan their moves out, and then proceed. It’s a necessary part of their lives, as they get older and we, as parents and their initial decision-makers, take a step back.
5. They build their interactive skills
Playing board games encourages a healthy, interactive relationship not only with their friends, but also with their parents. These are the social skills that will stay with them forever. 6. They teach children to follow instructions Games help with reading and, even more, with understanding and following through on directions. After all, a game can’t be played unless you’re making up the rules, which actually ties in with the next point.. 7. They massage their imagination I can recall several occasions when my children expanded on a game they were playing- changing the rules or even adding on to the game in a new way. I sometimes see pieces from one game on the board of another and smile to myself in satisfaction, after realizing they’ve tapped into their creativity to make up something new. 8. They keep them out of trouble This last one is a stretch, I know, but if you think this through, there’s definitely truth to the statement. All the while your kids are enjoying a good board game, they’re staying out of trouble. I count on the love my children have developed for this wonderful pastime in keeping them occupied for years to come. So go ahead, start a tradition that will be carried with them through the years, for their kids and their children’s kids and so on and so forth, trickling down the generations of healthy board game-lovers. About the author: Dana Corriel, MD, is a board-certified internist who writes regularly on her site drcorriel.com and runs her business: doctorsonsocialmedia.com. She has appeared in multiple publications, including the LA Times, Boston Globe, HuffPost, and SELF, and teaches healthcare professionals how to navigate through and optimize social media presence. Her favorite pastime is to explore other countries, which she does regularly, and writes about. 
By Jennifer Dawson
Oral diseases are health burdens for many countries affecting people, causing pain, and even death with more than 530 million children suffering from dental caries and cavities of milk teeth. Tooth decay and cavities can affect the life of a child big time. They cause pain, sleepless nights, missed days at school, poor appetite, and loss of interest in doing things that they like such as playing or hanging out with friends. In addition, tooth decay can be a sign of a poor diet which, in turn, leads to obesity and other conditions such as heart disease and type 2 diabetes. On the bright side, poor oral health is highly preventable. Apart from clinical interventions such as regular visits to the dentist, there are also day to day ways to complement an oral health plan for children.
Detecting the Signs of Dental Issues One of the first things to do in improving the oral health of kids is to be vigilant of the symptoms of caries and tooth decay caused by bacteria, among other things. Tooth decay can also be a result of food residues that contain sugars and starches left on the teeth. These may include milk, cereals, fruit juices, and bread, to name some. The combination of bacteria, saliva, food, and acid form plaque which sticks to the teeth of children. Moreover, a bacterial infection can also result in periodontal diseases in children, destroying the gums and supporting structures. For example, gingivitis, which is an inflammation of the gums, affects both children and adults. It is caused by the build up of plaque on the teeth and gum. Hence, it is vital to recognize the onset of periodontal diseases in children. As the gum disease is not generally painful, parents may not know that something is wrong. However, spotting the physical signs of the disease such as red and swollen gums, bleeding while brushing, receding gums, loose teeth, bad breath, and pus in between the teeth and gums help in early intervention. For evaluation and care, it is best to see a dentist to make a diagnosis. The treatment may include regular or deep cleaning by a dental hygienist antibiotics, and surgery, if the disease is at an advanced stage.
Integrated Oral Health Plan
In addition to clinical evaluations, it is important as well that children benefit from an integrated oral health plan. Once a diagnosis is confirmed, the dentist or periodontist can perform tooth extraction or surgery to correct gum problems. They may also put a dental sealant to prevent plaque build-up or apply fluoride to strengthen and protect enamel. However, non-clinical interventions are key to the success of an oral health care plan. Health, social, and education workers must have adequate understanding of child dental health to offer advice and refer parents and guardians to local services available. Schemes such as fluoride distribution programs in areas where fluoride is not present in the water systems, nutrition awareness and education specifically demonstrating the bad effects of sugar, and supervised toothbrushing projects in pre-schools can boost the dental health of children. Kids will also benefit enormously from the rigorous documentation and care of dentists and hygienists. Following up on treatments and preventive care will ensure good dental health. The bottom line is initiatives at the local level are effective in improving the oral health of kids. Moreover, integrating oral health in primary care services and implementing programs that work based on evidence indicate a good success rate. Poor oral health among children is a problem causing negative repercussions. The good news is in addition to clinical solutions, there are also non-medical interventions that help reduce cavities, tooth decay, and improve overall dental health among kids. About the Author: Jennifer Dawson is an experienced freelance writer with a particular interest in physical and mental health. She has previously worked in dental administration and when not working, she enjoys reading, traveling with her family and golf. 
By Cecile Bibawy
Since the publication of my book Loving Her Mind: Piecing Together the Shards of Hope, many people have shared with me their realization of the importance of opening up about their struggle upon discovering they are not alone. You can never tell your story in one go. Tell it a chapter at a time. Patients might significantly benefit from doctors and medical practitioners opening a “chapter” of a struggle they can share to open the communication about what might be going on. Alternatively, another’s story can be shared, like mine and the millions who struggle with mental illness. Keep the Secrets on the Playground If we stir up conversations about mental health and hardship, the secrets will lose their power, and those struggling will seek help. The only secrets left will be those whispered by the children on the playground. When we were children playing in the yards and swinging on the swings and climbing the monkey bars, we told secrets. It was thrilling to share secrets with my friend because it was information that was just for the two of us. As I grew, the secrets I kept were no longer from my friend but from my mother. Nostalgia grossly lacking, the information, just between the two of us, was sinister and downright impossible. When I was twelve or thirteen, my mother began telling me that certain relatives and classmates (my best friends) were psychopaths - evil agents of the devil who were out to get her. They were a threat to our family and we needed to stay far away from them. I was not permitted to tell anyone about these criminals because that would tip them off to the fact that she was aware of their evil and heighten the danger. I kept quiet. For six years, I told no one about my mother. Even after I finally realized at 16 that my friends and uncles were not evil and discovered that my mother suffered from schizophrenia, I didn’t speak about it. Because of the incessant verbal violence, paranoia, distrust, anger, and fear at home, and the isolation from friends and family, I wished throughout high school that an aunt or uncle or family friend would arrive to save my siblings and me from our misery.
When no one came, I began to silently satisfy myself with the idea of the county’s children’s services to whisk us away to a better life. Maybe then I’d have friends. Maybe I wouldn’t be so awkward. But that never happened. We were alone.
I don’t know if any of my schoolteachers, doctors, or Sunday school teachers knew about my mother. If they did, the subject was never discussed with me. I was fortunate that anytime I wanted, I could talk to my father about what was going on. But he was in survival mode the whole time that I was growing up and processing the monumental effects of my mother’s brain disease on me and the family. As her caregiver, he concentrated all efforts on maintaining her treatment, keeping her medicated, making sure our basic needs were met, and going to church. Resources were scarce - or we didn’t know of them. If there were support groups, counseling, or hotlines, we had no connections. I was never encouraged to talk about the silent monster called schizophrenia that roamed our home and infiltrated our lives in every imaginable way. And I was never asked.
In college, where I slowly started to open up to one or two trusted friends, new fears loomed. What if they don’t believe me? What if they laugh or scorn my words? What if they say I’m exaggerating or turn and run the other way? These fears were based on actual occurrences. So I remained quiet about my mother, my childhood, and mental illness and avoided bringing anyone to the house. My secrets were safe.
Our biggest secret - that we had mental illness in our family - practically wiped out the possibility of discovering resources for support. My parents placed a high importance on the opinions of the doctor. I doubt my mother’s psychiatrists gave my dad suggestions or resources for our family, like communication tools and coping strategies. If the family doctor or pediatrician had known what was going on, any information from them would have been taken seriously. This would have helped tremendously. It's a scary thing to talk about a personal encounter with mental illness - a thing marred with the unjust stains of blame, isolation, guilt, and shame. When we begin to tell our story, the walls shatter, the stigma dissipates, and hope is realized. We realize that we are not alone. We find someone kneeling beside us in our not-so-dark place helping us pick up the broken pieces. We all must tell our stories.
About the author: Cecile Bibawy spreads truth about mental illness, encourages people to tell their story for healing and stigma slaying, and promotes health of mind, body, and spirit. She homeschools her children with her husband in Sunbury, Ohio, and teaches fitness classes. Cecile is a speaker, teacher, and author. Connect with her at cecilebibawy.com, Facebook, Instagram (@sincerelycecile) and her favorite coffee shops. Loving Her Mind: Piecing Together the Shards of Hope is available for purchase at Amazon and Barnes & Noble.

By Kathleen O’Shea, Professor of English at Monroe Community College in Rochester, New York
At 55, my headache specialist, who had been a constant for me for 16 years--always there to help, encouraging me that if one medication or treatment didn’t work, we’d find another-- had retired, and I found myself in an intractable migraine cycle, which had already lasted for two months. I felt desperate, as there were/are few headache specialists in my area (Rochester, NY.), and they were over-booked already. I was lost, floundering, in pain, trying to keep working (teaching) at my best, but knowing something had to shift.
I decided to do what I’d always done when in pain (physical or psychological), and that was to turn to literature, since it invites the reader in to know he/she is not alone. In fact, I decided shortly after that, others needed to benefit from what I already knew: imaginative literature can give voice and insight into life experiences that find no outlet in any other way. The subjective and imaginative experiences that we often find difficult to describe, at least in ways that aren’t clinical and objective, are shared beautifully through poetry, fiction, plays, and non-fiction.
Literature taps another kind of resource for migraineurs and those seeking more understanding--the written testimony of essayists, fiction writers, poets, and dramatists, all who give eloquent, often passionate and harrowing accounts of multiple features of migraine that go beyond the pain of the fierce headache itself. The multiple sensations and symptoms of migraine, which capture the consuming pain, exhaustion, confusion, nausea, cognitive problems, and overwhelming fatigue and isolation that often accompany the disease, differs from patient to patient in some ways, but one of the predominant frustrations migraineurs share is a feeling that no one knows what migraine disease really feels like.
The migraine experience is often invisible because the symptoms, unlike a physical trauma, are often not apparent to a casual observer; the stigma remains. The migraineur attempts to function in his or her life and often becomes good at masking all of the other symptoms in order to achieve some measure of outward normalcy. People have trouble understanding how excessive yawning, confusion, irritability, crying, cognitive blanks, and heightened sensory awareness (smells, light) can all be attributed to a simple “headache.”
I knew, at this point, I needed to dig deeply to discover some of the best literature that could reach migraineurs in a number of ways: I chose the themes of the experience of migraine, the invisibility of migraine, the stigma that it’s just a headache, the reality that coping with this disease is a full-time, life-long job, and what migraineurs experience when it’s gone. In exploring these familiar themes migraineurs share, I developed a passion for learning about the disease, and, insofar as possible, “mastering” the condition through a self-understanding that I can share with readers. As a professor of literature, I have access to and have identified a large body of material on this subject that spans some four hundred years, from and 18th century poem to recently published novels, plays, and poetry.
Professionals in the field of migraine testify that there is a “hunger” for information on the subject, and while the internet and blogs can be useful, what they offer is often piecemeal and sometimes contradictory. I wrote So Much More than a Headache: Understanding Migraine through Literature, which provides an organized and sustained resource that is different in kind from other sources. Through contact with professional writers, migraineurs will find affirmation that they don’t experience this disease alone. Family, friends, and co-workers will better understand and empathize with the people they care about and work with.
Medical professionals and other groups trying to understand migraine will find in this anthology texts that can become invaluable starting points for discussion of the disease and the patients suffering with it. Finally, while I still suffer chronic migraine, I feel I am giving something to others. I have greatly benefited from researching and writing the book, and I hope to get it into the hands of whose who really need it. 
The 6 “Be's” of a good primary care visit
By Sully Cardona MD In the fast paced age we are living in today, it is common for physician visits to feel rushed. It can be hard to develop a good patient-doctor relationship. Patients have been sharing their dissatisfaction via patient surveys. I have been a family medicine physician for about 5 years at a local community health center. Here are some tips to get the most out of your primary care visits.
Be prepared: Write down your list of concerns: It’s easy to forget and be flustered when you’re face to face with your doctor. Do you need refills? If you don’t know the names and dosages of all the medicines you are taking, bring a list or your physical bottles. Are you having side effects from any of the medications? Is there a skin mole you’re concerned about? Or do you need tips on achieving a healthy weight?
Be understanding: Most appointment slots are scheduled for 15 minutes. That means that your doctor might not be able to get to all of your concerns. Be flexible and schedule more follow-up appointments to discuss your concerns. If you have several chronic medical conditions (such as diabetes or high blood pressure), be prepared for the doctor to spend the majority of the visit on these. Sometimes patients feel unheard when the doctor wants to spend more time focusing on their chronic medical conditions than their immediate concerns. Having a good relationship with your physician will help create trust and lead to more satisfying encounters. Be on time: If your appointment time is at 10 AM, that means you should be checked in and waiting to be called inside by 10 AM. Most practices have a 10-15 minute grace period, but remember that if every patient shows up 15 mins late, your appointment will be pushed back accordingly as your doctor tries to catch up. Be Flexible: as primary care doctors we literally have no idea what our day is going to look like. Since I’m a family medicine physician, I could have several easy, healthy, well child check-ups or I could have to disclose a new cancer diagnosis. Sometimes our electronic system stops working. There is nothing that stresses us out more than running behind, so please believe us when we say we work very hard to prevent this. If I have a new devastating diagnosis, I would want my doctor to take the time to answer my questions and offer some comfort.
Be proactive: Insurance is hard. Period. They change their coverage at the drop of a hat. They require pre-authorizations from one month to another. While we may be the only “face” you see in your medical encounter, please be aware that we have nothing to do with your insurance decisions. I encourage my patients to be proactive and call their insurance companies to find out what is covered, how much their copay will be etc.
Be healthy: Your doctor is going to tell you that you need to follow a healthy diet and exercise, sleep 7-8 hrs a night, and actively engage in stress-reducing activities. A lot of patients' health issues come from the lack of the above. Remember you might only see your doctor for 15 minutes several times a year, so it is up to you to take ownership of your health in between.
About the author: Sully Cardona MD is a board certified family medicine physician working in a community based health center for the last 5 years. Her interests include preventative care, family planning, procedures and lifestyle counseling. She is interested in helping patients become more proactive in their health. She earned a B.A in Chemistry from the University of Chicago, her M.D from the University of Illinois and completed her residency training at the Northwestern McGaw Family Medicine Residency Program. She is bilingual, fully fluent in Spanish. She likes to travel and play with her 2 younf daughters.
Invoke your spirit of volunteerism and add fun ways to stay mentally sharp as you age
By Sylvanus A. Ayeni, M.D.
While the actions of volunteers by and large do benefit the recipient(s), volunteerism also fosters wellness and wellbeing of the volunteer. Most of us, at some stage in our lives during and beyond adolescence, would probably think about the idea of volunteering for a good cause. The spirit of volunteerism, I believe is innate in all human beings, though it may be dormant in some people for varying lengths of time throughout their lives. There has been a plethora of research into various aspects of volunteerism. These aspects include motivation and its driving forces, commitment, altruism, the opportunity for social interactions and possible health benefits.
About the author:
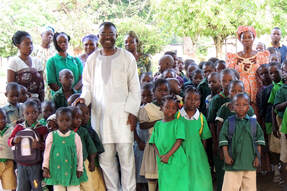
Sylvanus Ayeni is a retired neurosurgeon in the USA. He is President and Founder of Pan Africa Children Advocacy Watch, PACAW Inc. a non-profit organization involved in the education of children in Africa. He has been involved in development issues in Sub-Saharan Africa in the education and healthcare sectors for many years. |
Posts and advice from doctors to patients
|